Interventional Radiology: Techniques and Patient Benefits

What is Interventional Radiology and Its Purpose?
Interventional radiology (IR) is a medical specialty that utilizes imaging techniques to guide minimally invasive procedures. This innovative approach allows doctors to diagnose and treat various conditions without the need for traditional surgery. By employing tools like X-rays, CT scans, and ultrasounds, IR specialists can perform interventions with pinpoint accuracy, reducing risks and recovery times.
Interventional radiology is a medical specialty that uses imaging techniques to guide minimally invasive procedures, revolutionizing treatment options for patients.
The primary purpose of interventional radiology is to provide effective treatments for conditions such as blood vessel blockages, tumors, and internal bleeding. By using small incisions and specialized instruments, patients often experience less pain and a quicker return to their daily activities. This shift from open surgery to IR techniques is revolutionizing how many medical conditions are managed.
As a result, interventional radiology is a game-changer in the healthcare field, offering patients alternatives that are not only safer but also more efficient. With a focus on patient-centered care, IR specialists aim to improve outcomes while minimizing discomfort. This specialty continues to evolve, bringing new techniques and technologies to the forefront of modern medicine.
Common Techniques Used in Interventional Radiology
Interventional radiology encompasses a variety of techniques, each tailored to specific medical needs. Some of the most common methods include angioplasty, where a balloon is used to open narrowed blood vessels, and stenting, which involves placing a small mesh tube to keep the vessel open. Other techniques include embolization, used to block blood flow to certain areas, and ablation, which destroys abnormal tissue using heat or cold.
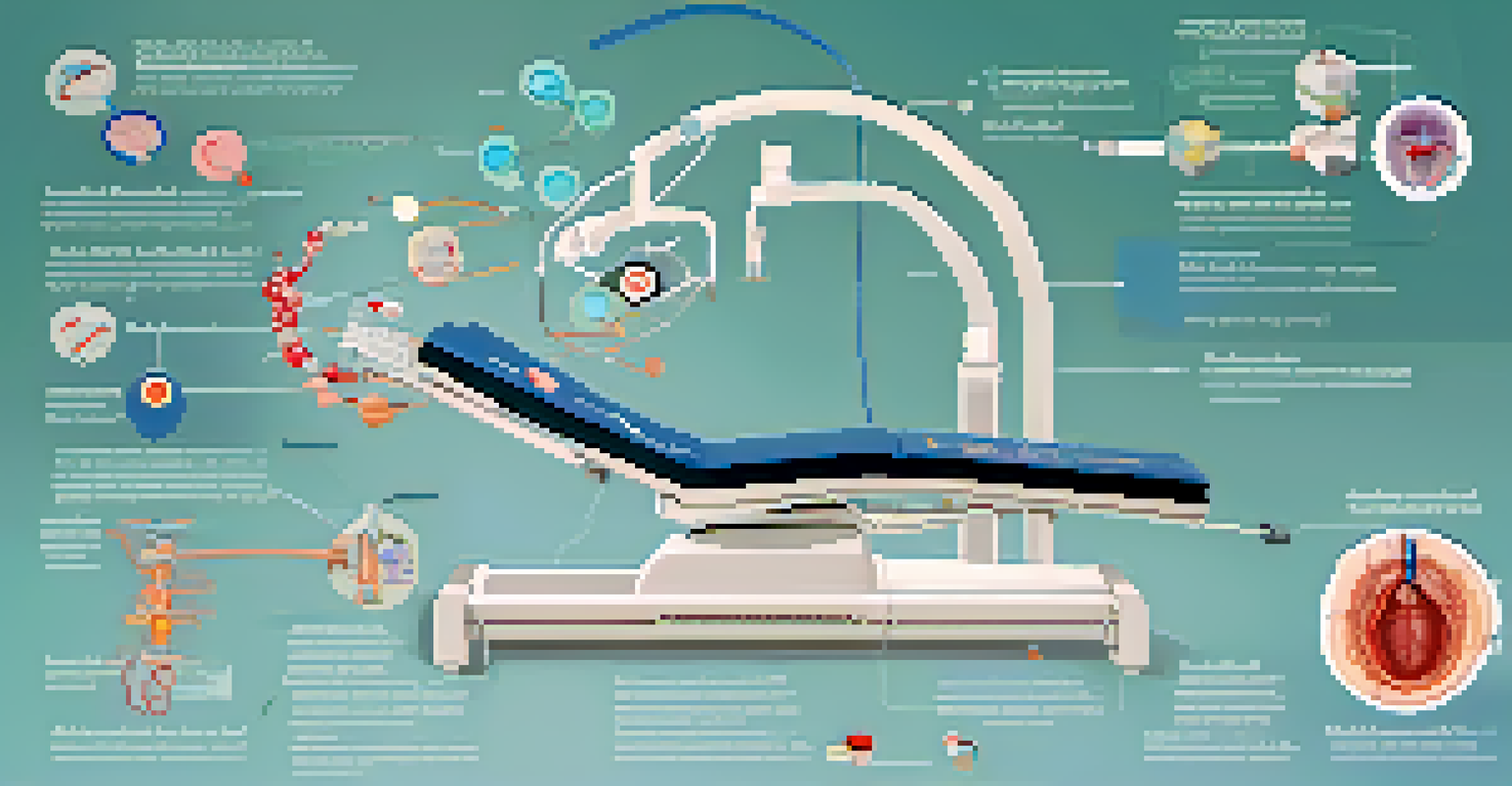
These procedures are typically performed in a hospital or outpatient setting, ensuring patient comfort and convenience. They are often guided by real-time imaging, allowing physicians to navigate to the exact location of the issue with precision. This level of accuracy not only enhances the effectiveness of the treatment but also minimizes damage to surrounding tissues.
Minimally Invasive Procedures
Interventional radiology provides effective treatments through small incisions, reducing pain and recovery time.
In addition to these techniques, interventional radiologists are continually developing new methods to address complex medical challenges. Innovations such as catheter-directed therapy and image-guided biopsies are expanding the possibilities of what can be achieved through IR. As technology advances, patients can expect even more effective treatments with fewer complications.
Benefits of Interventional Radiology for Patients
One of the standout benefits of interventional radiology is its minimally invasive nature. Unlike traditional surgical methods, which often require large incisions, IR procedures typically involve only small punctures, leading to reduced pain and faster healing times. This aspect is particularly appealing to patients who wish to avoid prolonged hospital stays and lengthy recovery periods.
The integration of advanced imaging technology in interventional radiology ensures precision, enhancing the effectiveness of procedures while minimizing risks.
Additionally, many interventional radiology procedures can be performed on an outpatient basis, allowing patients to return home the same day. This convenience not only improves the overall patient experience but also helps reduce healthcare costs. With less time spent in the hospital, patients can focus on their recovery in the comfort of their own homes.
Moreover, interventional radiology often leads to fewer complications compared to open surgery. The precision of imaging-guided techniques minimizes the risks of infection and other adverse effects. As patients increasingly seek safer and more effective treatment options, interventional radiology is proving to be a reliable choice in modern medicine.
Patient Safety and Interventional Radiology
Patient safety is paramount in interventional radiology, and various protocols are in place to ensure a secure environment. Before any procedure, thorough assessments and consultations are conducted, allowing the medical team to understand the patient’s history and potential risks. This careful planning helps tailor each intervention to the individual’s needs.
During procedures, advanced imaging technology plays a crucial role in enhancing safety. By providing real-time visuals, doctors can monitor the procedure closely and make adjustments as needed. This continuous oversight significantly reduces the likelihood of complications, giving patients and their families peace of mind.
Advanced Imaging Techniques
Imaging technology like X-rays and ultrasounds are essential in guiding interventional radiology procedures with precision.
Post-procedure care is also a vital component of patient safety. Interventional radiologists provide clear instructions on recovery and potential side effects, ensuring patients are informed throughout their healing journey. By prioritizing safety at every stage, interventional radiology fosters a trusting relationship between patients and their healthcare providers.
Conditions Treated by Interventional Radiology
Interventional radiology is versatile and can address a wide range of medical conditions. Common issues treated include vascular diseases, such as peripheral artery disease, where blood flow to the limbs is restricted. Additionally, IR is effective for treating tumors in various organs, using techniques like ablation to destroy cancerous tissues while sparing healthy ones.
Other conditions that benefit from interventional radiology include gastrointestinal bleeding, bile duct obstructions, and kidney stones. The ability to perform targeted interventions allows for effective management of these issues without resorting to invasive surgical procedures. This versatility makes IR an essential component of modern healthcare.
As research and technology continue to advance, the scope of conditions treated by interventional radiology is expanding. Innovations are leading to new applications, such as treating chronic pain and managing conditions related to obesity. This continuous evolution ensures that more patients can benefit from the innovative techniques offered by interventional radiologists.
The Role of Imaging in Interventional Radiology
Imaging technology is the backbone of interventional radiology, guiding procedures and ensuring precision. Techniques such as fluoroscopy, which provides real-time X-ray visuals, and ultrasound imaging are commonly used to navigate during interventions. These tools are essential for identifying the exact location of medical issues and determining the best course of action.
The accuracy provided by imaging not only enhances the effectiveness of procedures but also minimizes the risk of complications. By allowing doctors to visualize internal structures clearly, imaging helps avoid damage to healthy tissues. This focus on precision is particularly important in delicate areas, such as near vital organs and blood vessels.
Evolving Treatment Options
The field of interventional radiology is continuously advancing, offering new and personalized approaches to a wide range of medical conditions.
As imaging technology continues to advance, interventional radiology is likely to see even greater improvements in safety and outcomes. Innovations such as three-dimensional imaging and advanced computer algorithms are paving the way for more effective interventions. In this evolving landscape, the role of imaging remains critical to the success of interventional radiology.
Future Trends in Interventional Radiology
The future of interventional radiology is bright, with ongoing advancements promising to enhance patient care further. One significant trend is the integration of artificial intelligence (AI) into imaging and procedural planning. By analyzing vast amounts of data, AI can assist doctors in making more informed decisions and improving procedural outcomes.
Another exciting development is the growth of personalized medicine within interventional radiology. Tailoring treatments to the individual characteristics of patients—such as genetics and lifestyle—can lead to more effective interventions. This shift toward patient-specific approaches is likely to revolutionize how conditions are treated in the coming years.

Additionally, the continued refinement of techniques and technologies will expand the range of conditions that can be effectively managed through interventional radiology. As more minimally invasive options become available, patients will benefit from safer, quicker, and more effective treatments. This evolution ultimately reinforces interventional radiology's vital role in the future of healthcare.