B Cells and Antibody Production: Key Players in Immunity
Understanding B Cells: The Immune System's Architects
B cells are a type of white blood cell that play a crucial role in our immune system. They originate from bone marrow and are essential for producing antibodies, which help identify and neutralize pathogens like bacteria and viruses. Think of B cells as architects of our immune response, designing the blueprints that help our body recognize invaders.
The immune system is a complex network of cells and proteins that defends the body against infection. B cells are a crucial part of that system, acting as the architects of our immune response.
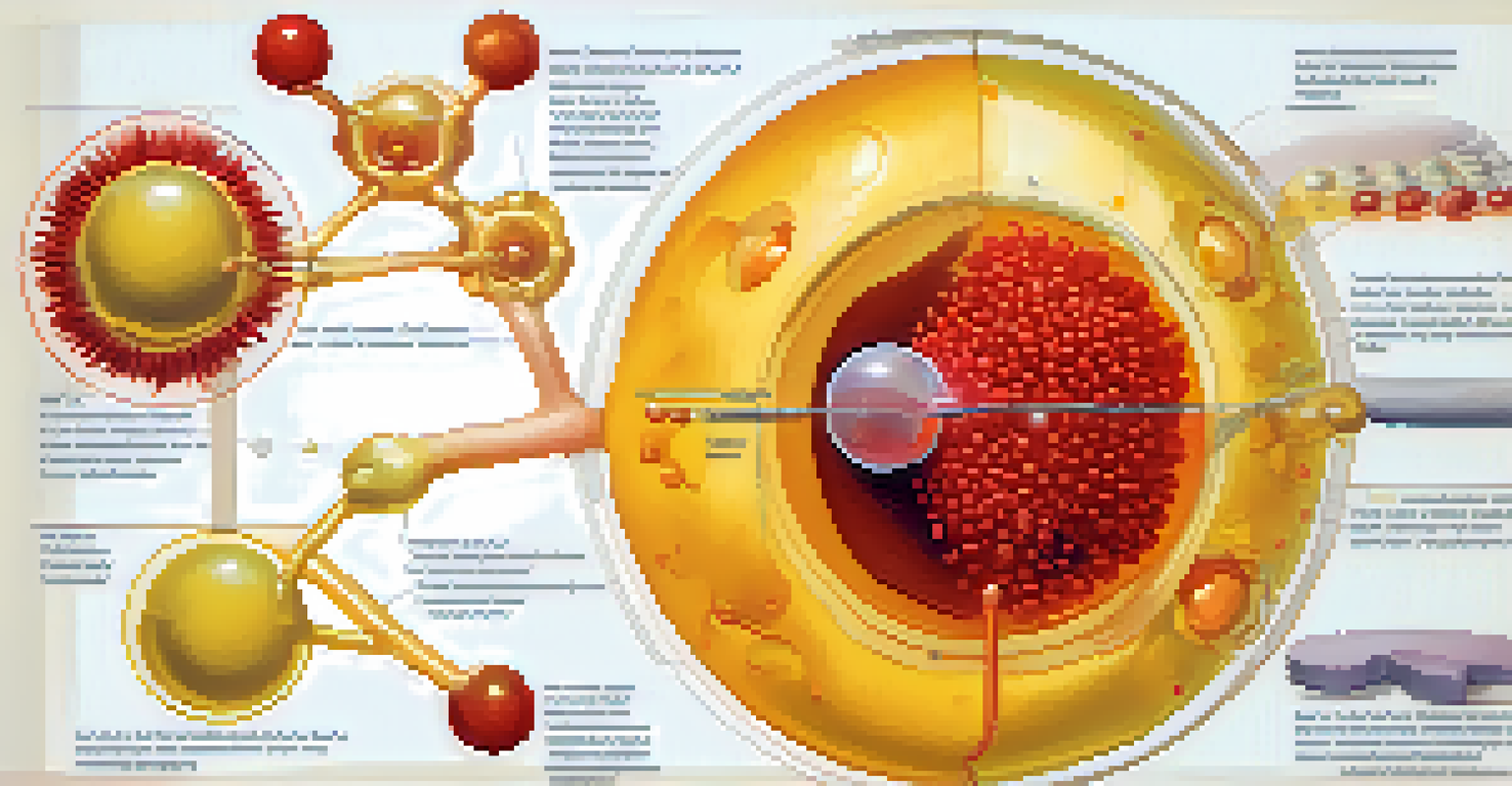
Once activated by encountering an antigen, a foreign substance that triggers an immune response, B cells undergo a transformation. They proliferate and differentiate into plasma cells, which are like factories pumping out antibodies. This process is vital because it equips our body with the tools needed to fight off infections effectively.
In addition to producing antibodies, B cells also develop a memory of the encountered pathogens. This means if the same invader tries to attack again, the immune system can respond more rapidly and efficiently. It's like having a library of blueprints that allows your body to quickly recognize and tackle familiar foes.
Antibodies: The Body's Specialized Defense Weapons
Antibodies, also known as immunoglobulins, are Y-shaped proteins produced by B cells. They have a unique ability to bind to specific antigens, much like a lock and key mechanism, which helps neutralize or mark invaders for destruction. This specificity is what makes antibodies so powerful in our immune defense.
There are five main classes of antibodies—IgG, IgA, IgM, IgE, and IgD—each with distinct roles. For example, IgG is the most abundant and plays a key role in long-term immunity, while IgE is primarily involved in allergic reactions. This diversity ensures that our immune system can tackle a wide range of threats effectively.
B Cells Create Immunity Blueprints
B cells produce antibodies and develop memory, enabling the immune system to recognize and respond to pathogens efficiently.
When antibodies bind to pathogens, they can neutralize them directly or tag them for destruction by other immune cells. This process is akin to putting a 'wanted' poster on the pathogen, making it easier for the body to eliminate it. The versatility of antibodies is a cornerstone of our body's defense strategy.
Activation of B Cells: The First Step in Immune Response
The activation of B cells is a critical first step in mounting an immune response. This process often begins when B cells encounter an antigen that fits their unique receptors. Once they bind to the antigen, they require additional signals from helper T cells to fully activate and start the antibody production process.
Vaccination is the most effective way to prevent infectious diseases, as it primes the immune system to recognize and combat pathogens swiftly, thanks to the memory B cells that are formed.
This collaboration between B cells and T cells illustrates the interconnectedness of our immune system. Think of it as a team effort, where each player has a specific role that contributes to the overall success of the immune response. Without these signals, B cells may remain dormant and unable to fulfill their protective function.
Once activated, B cells can proliferate rapidly and differentiate into effector cells. This is when they begin producing large quantities of antibodies, gearing up for battle against the invading pathogens. The efficiency of this activation process is vital for a robust immune response.
Memory B Cells: The Guardians of Long-Term Immunity
After an infection has been cleared, some B cells don’t just disappear; they become memory B cells. These specialized cells are like seasoned veterans of the immune system, ready to spring into action if the same pathogen reappears. This memory is what provides long-term immunity and is the principle behind vaccines.
Memory B cells can live for years, even decades, allowing for a quicker and more effective response to previously encountered pathogens. When exposed again, they can rapidly convert into plasma cells to produce antibodies more efficiently than during the first encounter. This rapid response is crucial in preventing reinfection.
Vaccines Leverage B Cell Function
Vaccines stimulate B cells to produce antibodies and memory cells, training the immune system to combat future infections effectively.
This mechanism is why vaccines are so effective. By training the immune system to recognize a harmless version of a pathogen, vaccines prepare memory B cells to respond swiftly if the actual pathogen is encountered in the future. It's a brilliant strategy that enhances our immunity and protects us from disease.
The Role of B Cells in Autoimmune Diseases
While B cells are essential for protecting us from infections, they can sometimes misfire, contributing to autoimmune diseases. In these conditions, B cells mistakenly produce antibodies against the body's own tissues, leading to inflammation and damage. It's like a miscommunication in a team, where instead of defending the team, they turn against their own players.
Common autoimmune diseases, such as lupus and rheumatoid arthritis, often involve an overactive B cell response. Understanding the mechanisms behind this misactivation is crucial for developing targeted therapies. By identifying the triggers, researchers can work on strategies to prevent B cells from attacking healthy cells.
The balance between an effective immune response and avoiding autoimmunity is delicate. Ongoing research aims to fine-tune our understanding of B cell behavior to harness their protective capabilities while minimizing the risk of autoimmunity. This is key to advancing treatments and improving patient outcomes.
The Impact of Vaccines on B Cell Function
Vaccines are a prime example of how we can leverage B cell function to bolster immunity. By introducing a harmless component of a pathogen, vaccines stimulate B cells to produce antibodies and create memory cells without causing disease. This process essentially trains the immune system, preparing it for future encounters with the real pathogen.
For instance, the flu vaccine prompts the body to recognize and fight off the flu virus more effectively. Each year, as the virus evolves, researchers update the vaccine to match the circulating strains, ensuring our B cells are prepared. This adaptability highlights the importance of B cells in our ongoing fight against infectious diseases.
B Cells and Autoimmune Challenges
While vital for defense, B cells can contribute to autoimmune diseases by mistakenly attacking the body's own tissues.
The success of vaccines underscores the significance of B cells in public health. By increasing herd immunity through widespread vaccination, we protect not only ourselves but also those who may be more vulnerable, such as infants and the elderly. This collective defense showcases the power of B cells in safeguarding our communities.
Future Research: Enhancing B Cell Responses for Better Health
The study of B cells and their role in immunity continues to evolve, with researchers exploring new ways to enhance their responses. Advances in immunotherapy aim to boost B cell function, which could lead to better treatments for infections and autoimmune diseases alike. This research could redefine how we approach various health challenges.
Emerging technologies, such as gene editing and personalized medicine, hold promise for tailoring B cell responses to individual needs. By understanding a person's unique immune profile, scientists can develop targeted therapies that optimize B cell activity. This personalized approach could revolutionize patient care and improve outcomes.
As we delve deeper into the complexities of the immune system, the potential for enhancing B cell responses offers exciting possibilities. Whether it's creating more effective vaccines or developing novel treatments for autoimmune diseases, the future of B cell research is bright and full of promise.