Dermatitis: Types, Symptoms, and Effective Treatment Options

What is Dermatitis? An Overview of the Condition
Dermatitis is a general term for inflammation of the skin. It often presents as red, itchy patches that can be uncomfortable and unsightly. While it can affect anyone, certain factors like genetics and environmental triggers can increase susceptibility. Understanding the fundamentals of dermatitis is crucial for effective management and treatment.
The skin is the mirror of the body. If you want to find out what is going on inside, you need to look at the skin.
This skin condition can manifest in several forms, each with unique characteristics and causes. While some types may stem from allergies, others may be linked to irritants or even stress. Identifying the type of dermatitis you have is essential for finding the right treatment and alleviating symptoms.
Ultimately, dermatitis can significantly impact one's quality of life. It's not just a cosmetic issue; the discomfort can interfere with daily activities and emotional well-being. Recognizing the signs and symptoms early can help in seeking appropriate care.
Common Types of Dermatitis: A Closer Look
There are several common types of dermatitis, including atopic dermatitis, contact dermatitis, and seborrheic dermatitis. Atopic dermatitis, often associated with allergies and asthma, is characterized by dry, itchy skin. Contact dermatitis occurs when the skin reacts to irritants or allergens, leading to redness and inflammation.
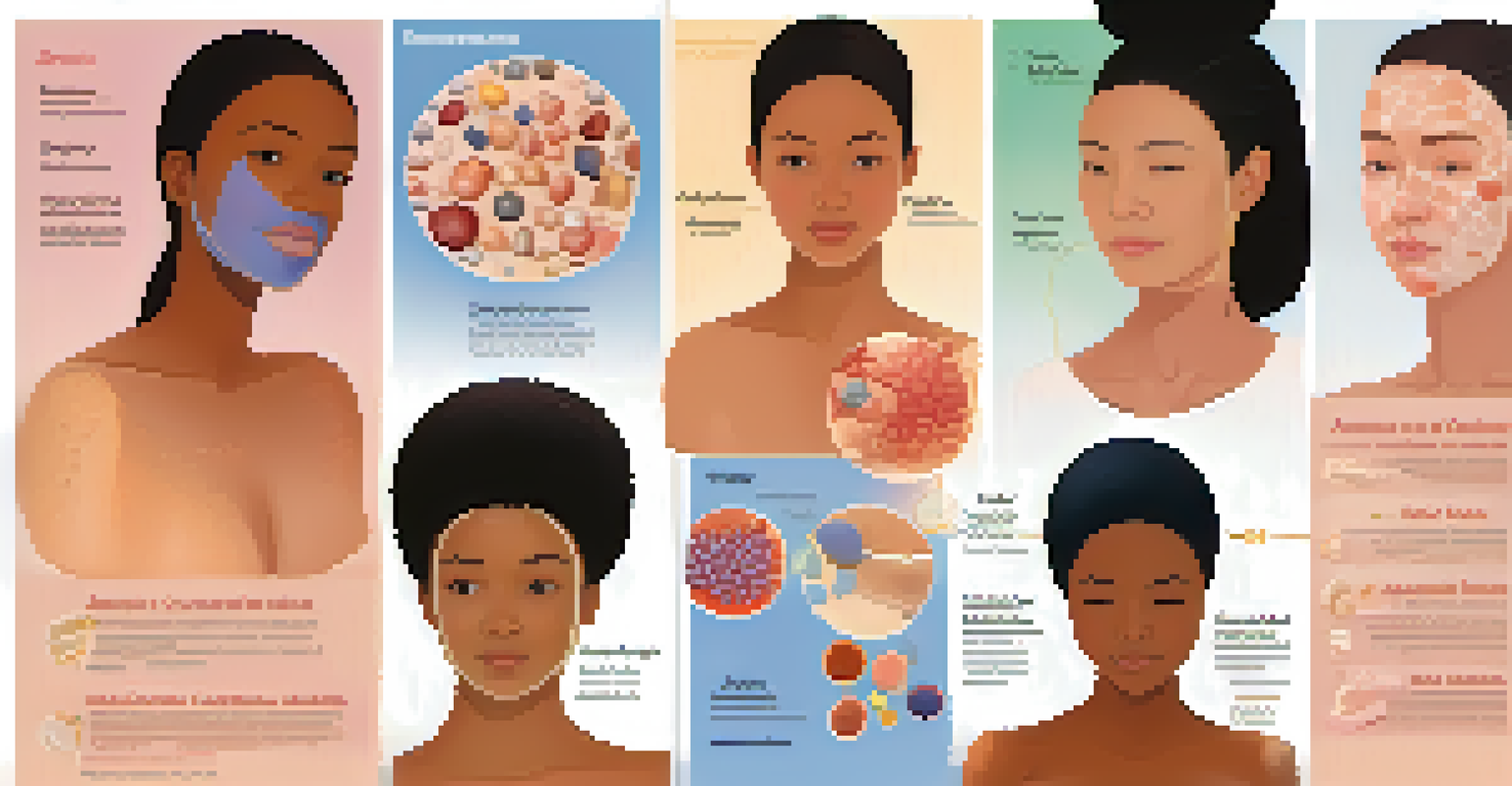
Seborrheic dermatitis primarily affects the scalp, causing dandruff and oily, flaky patches. It can also appear on the face and other oily areas of the body. Each type has its unique triggers and symptoms, making it important to understand which form of dermatitis you might be dealing with.
Understanding Dermatitis Basics
Dermatitis is an inflammatory skin condition characterized by red, itchy patches and can significantly affect quality of life.
It's also worth mentioning that dermatitis can vary in severity and duration. Some people might experience acute flare-ups, while others may have chronic issues that require ongoing management. Recognizing these differences can aid in better treatment planning.
Symptoms of Dermatitis: What to Watch For
The symptoms of dermatitis can vary widely depending on the type and severity of the condition. Common signs include red, inflamed skin, itching, and dryness. In some cases, blisters or crusty patches may develop, which can lead to further discomfort and potential infections.
Your skin is your best accessory. Take good care of it.
Often, the itching associated with dermatitis can be intense, leading to scratching that exacerbates the condition. This cycle of itching and scratching can make it difficult to find relief and can prolong the healing process. It’s essential to avoid scratching to prevent further irritation.
Additionally, some individuals may notice that their symptoms worsen in response to specific triggers, such as certain foods, fabrics, or environmental factors. Keeping a journal of flare-ups can help in identifying these triggers and managing symptoms more effectively.
Causes of Dermatitis: What Triggers the Condition?
Dermatitis can arise from several different causes. Allergens, such as pollen, pet dander, or certain foods, can trigger atopic dermatitis. Contact dermatitis, on the other hand, is often linked to exposure to irritants like soaps, detergents, or chemicals found in cosmetics.
Genetic factors can also play a role, especially in conditions like atopic dermatitis. If you have a family history of allergies or skin conditions, it may increase your risk of developing dermatitis. Environmental factors, including humidity and temperature, can further exacerbate symptoms.
Types and Symptoms of Dermatitis
Common types of dermatitis, including atopic and contact dermatitis, present with various symptoms like redness, itching, and dryness.
Lastly, lifestyle factors such as stress or lack of sleep may contribute to flare-ups. Managing stress through relaxation techniques or regular exercise can help in reducing the likelihood of dermatitis outbreaks.
Diagnosis of Dermatitis: How is it Identified?
Diagnosing dermatitis typically begins with a thorough examination by a healthcare professional. They will assess your skin and inquire about your symptoms, medical history, and any potential triggers. This discussion can provide valuable insights into the type of dermatitis you may have.
In some cases, additional tests may be necessary to pinpoint the exact cause of the condition. These may include patch testing for contact dermatitis or allergy testing to identify specific allergens. Understanding the underlying cause is critical for developing an effective treatment plan.
Don't hesitate to seek a second opinion if you're uncertain about your diagnosis. Accurate identification is vital, as different types of dermatitis may require different approaches to treatment.
Effective Treatment Options for Dermatitis
Treatment for dermatitis often starts with over-the-counter creams or ointments to soothe the skin and reduce inflammation. Hydrocortisone cream is a common choice for mild cases, while stronger prescription treatments may be necessary for more severe cases. Moisturizers also play a crucial role in keeping the skin hydrated and preventing flare-ups.
In cases of contact dermatitis, identifying and avoiding the irritant or allergen is essential for effective treatment. This might involve changing personal care products or altering daily routines. For atopic dermatitis, lifestyle changes like stress management can also be beneficial.
Effective Management Strategies
Managing dermatitis involves identifying triggers, utilizing appropriate treatments, and maintaining a consistent skincare routine.
In some instances, oral medications or phototherapy may be recommended by a healthcare provider. It's essential to follow their guidance and regularly monitor your symptoms to adjust your treatment plan as needed.
Preventive Measures: How to Manage Dermatitis
Managing dermatitis requires a proactive approach to prevent flare-ups. This includes identifying and avoiding known triggers, whether they be allergens, irritants, or stressors. Developing a consistent skincare routine with gentle products can also help maintain skin health.
Wearing breathable fabrics and avoiding harsh chemicals in cleaning products can reduce irritation. Additionally, keeping your living environment clean and free of dust can mitigate allergy-related flares. Consistency in your preventive measures is key to long-term management.

Lastly, staying informed about your condition and potential treatment options can empower you in your journey. Regular check-ins with a healthcare professional can help you adjust your management plan as needed and provide support.